Just released: Two new reports on injury prevention in BC

A new economic report shows that injuries cost British Columbia $3.7 billion in one year. The Economic Burden of Injury in British Columbia, published today by the BC Injury Research and Prevention Unit (BCIRPU), shows where injury prevention efforts could have the greatest return on investment for all age groups. The dollars include health care system costs, such as hospitalization and patient care expenses, as well as indirect costs of lost economic productivity from disability and premature death.
To support communities, BCIRPU produced the British Columbia Casebook of Injury Prevention, a highly visual, online resource with useful charts and info graphics that help make the case for injury prevention. The Casebook includes nine high quality examples of injury prevention in action from the health authorities and demonstrates positive return on investment in injury prevention initiatives.
Please click on the following link for both new resources: the BC Casebook for Injury Prevention and the Economic Burden of Injury in BC.
The Economic Burden of Injury in British Columbia was supported by the BC Ministry of Health, the Child & Family Research Institute (CFRI), the Provincial Health Services Authority, and the University of British Columbia. The report is based on the latest available data (2010) from the BC Ministry of Health, BC Vital Statistics, National Ambulatory Care Reporting System and Statistics Canada as well as calculations for disability rates and morbidity costs. The costing methodology for this internationally peer reviewed report is based on Parachute’s Electronic Resource Allocation Tool, combining existing data with variables from the literature in order to model the full costs of unintentional and intentional injuries.
The British Columbia Casebook of Injury Prevention was supported by the Provincial Health Services Authority, Fraser Health, Interior Health, Island Health, Northern Health, Vancouver Coastal Health, First Nations Health Authority and Parachute Canada.
If you are interested in helping to evaluate the BC Casebook for Injury Prevention, please click here.
The BC Injury Research and Prevention Unit is supported by the Child & Family Research Institute, BC Children’s Hospital Foundation, BC Ministry of Health, Provincial Health Services Authority, and the University of British Columbia.
If you have any questions, please contact us at bcinjury1@cw.bc.ca. We look forward to hearing from you.
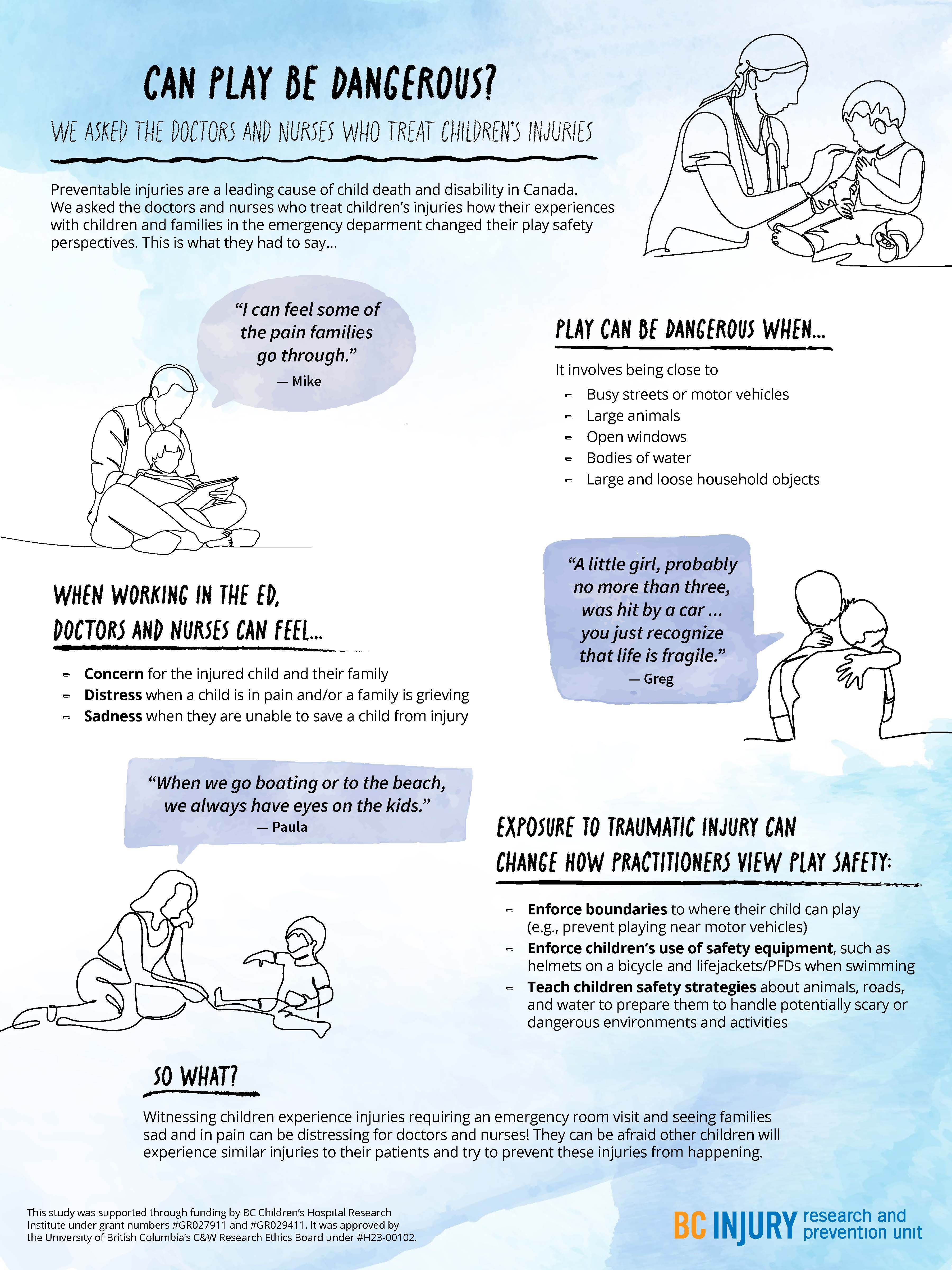
- distress when a child was in pain and when a family was grieving; and
- sadness in the event they were not able to save a child in their care.
- concern for the injured child and the child’s family;
Particularly traumatic events, such as those involving vivid sights and sounds (e.g., families holding each other and having extreme reactions), stuck with the practitioners, having long-lasting impressions on them and causing them to re-live these events in the years following their exposure.
Even after their shift was over, practitioners said that they changed how they approached parenting and how they perceived safety during play as a result of witnessing these traumatic events. They reported having more knowledge of the causes and consequences of severe injuries, such as those that require hospitalization or emergency care. For example, practitioners were more likely to enforce boundaries around where their children could play, such as by forbidding their child to play near busy streets. They also were more likely to tell their child about safe play environments and equipment, and put this equipment on their child before play, such as explaining the benefits of using helmets while riding bikes.
Practitioners were more likely to enforce boundaries around where their children could play, and use safety equipment, such as bike helmets.
Practitioners also described being concerned about their children’s play near open windows, around large bodies of water unsupervised, and in environments where firearms were present. They also expressed worry about their children’s play on trampolines and on motorized vehicles, such as ATVs. Findings related to trampoline play safety concerns were published in the journal Injury Prevention.
Observing family grief due to child injury or death affected the mental well-being of health care practitioners, drawing attention to the need for mental health supports for those involved in caring for severely injured and dying patients.

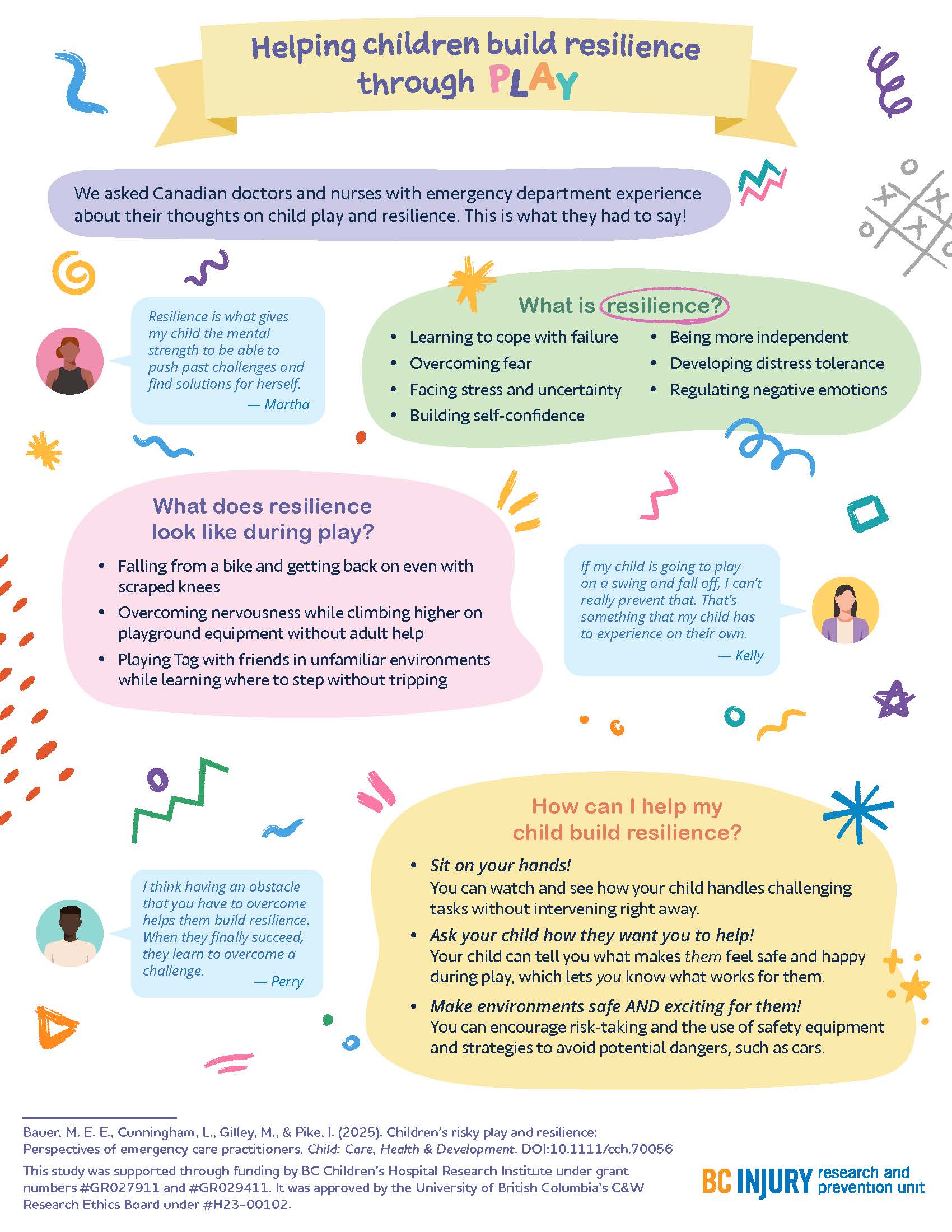
"Raise more resilient children through play...watch and see how your child handles challenging tasks without intervening right away." —Dr. Michelle Bauer
Building resilience through play
How can parents help their children build resilience? By letting them play!
The experiences that practitioners witnessed encouraged them to support their children in building resilience through play; specifically, by supporting children in learning to cope with failure, overcome fear, build self-confidence, develop distress tolerance, and regulate negative emotions. Findings related to building resilience through play were published in the journal Child: Care, Health, and Development.

Parents fostered resilience in their kids by:
- helping their kids get back on bikes after they fell off and wanted to try again;
- sitting on their hands so they did not instinctively reach for their children when their children fell down; and
- encouraging participation in challenging and thrilling activities in forests and water while safety equipment was used.
"There are a few ways that parents can raise more resilient children through play that are supported by literature and our study findings," said Dr. Bauer. "One: watch and see how your child handles challenging tasks without intervening right away."
"Two: Ask your child how they want you to help—let them tell you what makes them feel safe and happy during play. Let them lead. And three: make play both safe and exciting by encouraging risk-taking, teaching them how to avoid hazards, and using safety equipment.”
This research was supported through Drs. Bauer’s and Gilley’s receipt of a clinical and translational research seed grant from the BC Children’s Hospital Research Institute (BCCHR), Dr. Bauer’s BCCHR postdoctoral fellowship award, and additional training provided to Dr. Bauer through her participation in the Programs and Institutions Looking to Launch Academic Researchers (PILLAR) program through ENRICH, a national organization training perinatal and child health researchers.
Learn more about the study through two infographic posters:
Graphics and posters by Milica Radosavljevic