Injury Insights: Research (December 2025)

The third edition of our Injury Insights: Research series highlights a selection of recent publications by BCIRPU researchers.
Comparing pedestrian and cyclist injuries from falls and collisions in British Columbia, Canada: Frequencies and population characteristics (June 2025)
Authors: Michael Branion-Calles, Andrea Godfreyson, Kate Berniaz, Neil Arason, Shannon Erdelyi, Meghan Winters, Kay Teschke, Fahra Rajabali, M. Anne Harris, Jeffrey R. Brubacher
This study aims to highlight the emerging evidence that injuries from pedestrian and cyclist falls occur more frequently than collisions with motor vehicles, despite the former often being omitted from traditional road safety data sets. Quantitative hospital admissions data were used to compare the frequency, injury severity, and population characteristics of pedestrians and cyclists who have been injured from falls versus collisions.
For both pedestrians and cyclists, collisions with motor vehicles had a higher proportion of severe injuries than falls, but pedestrian and cyclist falls were much more frequent. Falls disproportionately affected older adults, females, higher-income individuals, and rural residents. These findings show that falls are major contributors to the burden of road traffic injury, and therefore should be included in road safety surveillance and research in order to improve road safety for pedestrians and cyclists.
Read more in the Journal of Transport & Health.
Underreporting and selection bias of serious road traffic injuries in auto insurance claims and police reports in British Columbia, Canada (March 2025)
Authors: Michael Branion-Calles, Andrea Godfreyson, Kate Berniaz, Neil Arason, Herbert Chan, Shannon Erdelyi, Meghan Winters, Joy Sengupta, Mohamed Essa, Fahra Rajabali, Jeffrey R. Brubacher
Much of road safety research conducted is based on administrative data, including police reports, insurance claims, and medical records that are prone to under-reporting and selection bias. This study assessed these biases and examined the overlap of serious road traffic injuries involving motor vehicles across multiple injury datasets in British Columbia from 2015 to 2019.
Using probabilistic linkage, the study connected police reports, insurance claims, and hospital admissions to a provincial population directory to identify distinct persons and injuries. Additional sociodemographic and geographic details were linked to injuries from other government sources. Analyses focused on serious injuries to drivers, cyclists, and pedestrians, assessing both the proportion of injuries captured by a database – the ascertainment rate – and selection bias among groups most likely to only be captured in hospital admissions.
An estimated 57,097 motor vehicle-involved injuries were found from 2015 to 2019, with 48,198, 2,641, and 6,258 injuries being from motor vehicle drivers, cyclists, and pedestrians, respectively. The ascertainment rate was highest for drivers (95.7%) and lower for cyclists (83.3%) and pedestrians (76.5%) in insurance data. Results showed that police records and hospital admissions better captured pedestrian and cyclist injuries than driver injuries. Unlinked injuries in the hospital admissions data were typically from low-income and remote populations.
This underreporting underscores the need for improved injury surveillance for pedestrians and cyclists to better represent the burden of injury, particularly among marginalized sociodemographic groups.
Read more in the journal Transportation Research Interdisciplinary Perspectives.
Evidence-Informed Quality Indicators for Pediatric Trauma Care (June 2025)
Authors: Lynne Moore, Ian Pike, Natalie Yanchar, Pier-Alexandre Tardif, et al
There is a lack of quality indicators (QIs) to support quality improvement in the pediatric trauma patient population, despite their unique characteristics and health care needs. A modified Research and Development (RAND)/University of California Los Angeles (UCLA) expert consensus study involving 59 participants was conducted, with the goal of developing a set of QIs for acute pediatric trauma care. This involved an online survey component, where the experts were presented QIs and asked to rate them on a 7-point Likert scale according to a provided set of criteria. This portion was then followed by a virtual workshop in which the experts engaged in facilitated discussion until consensus was achieved.
23 QIs were identified, including improvements to effectiveness, safety, cost-effectiveness, equity, and a patient-centred approach. These QIs may further be used to develop other context-specific QIs, and measure and improve adherence to guideline recommendations on pediatric trauma management.
Read more in the journal JAMA Pediatrics.
“If a shoe had been designed from a woman’s foot, would I be running without getting the injuries?”: running footwear needs and preferences of recreational and competitive women runners across the lifespan (October 2025)
Authors: Christopher Napier, Gurmeet Dhillon, Anna-Catharina Wilhelm, Allison M. Ezzat
Currently, most running footwear is designed and tested for males/men, despite known sex and gender differences between males/men and females/women. This study involved focus groups with 21 women runners of different ages, running experience, and running volume to understand their needs and preferences for running footwear and how these can change across the lifespan.
This study highlights how women’s footwear needs are often unmet. Using qualitative methods, researchers found that women value running shoes that prioritize comfort and feel, seek different shoe options for different running contexts, and want a clear understanding of how footwear contributes to injury prevention. These needs were found to change across the lifespan, such as increasing shoe width during pregnancy/postpartum and having greater stability and cushioning with age.
Given the strong belief in the role of footwear in injury prevention among women, more evidence-based education on this topic is needed. These findings call for the design of running shoes that better meet unique needs of women, regardless of their participation level, and enhance running performance, comfort, and injury prevention.
Read more in the journal BMJ Open Sport and Exercise Medicine.
Parental perspectives of physicians and nurses on child trampoline use: “I feel like I’m just kind of caving to social pressure” (June 2025)
Authors: Michelle E.E. Bauer, Meghan Gilley, Ian Pike
Despite evidence on the risk of injury associated with trampoline use among children, trampoline jumping remains a popular activity. For this study, researchers used interviews to explore the perspectives of parents who are emergency practitioners (physicians and nurses) regarding their children’s trampoline use.
Themes identified included having heightened awareness for injury due to working with patients in emergency departments; feeling social stigma if they allow their children to use trampolines; and the need to balance healthy child development through exciting activities such as jumping while keeping children safe from being injured. Findings from the study show that parents' decisions for encouraging or restricting their children's trampoline use can be influenced by witnessing trampoline-related injuries and having access to injury information and health education.
Read more in the journal Injury Prevention.
Workplace concussion recovery is everyone’s responsibility (July/August 2025)
Authors: Shelina Babul, Karen Takai, Olivia Sampson
In 2023, WorkSafeBC data reported 2,754 work-related concussion claims that required ongoing benefits. Concussion symptoms can persist beyond four weeks in approximately one in six adults. An early, evidence-based approach to diagnosis and management is important to support injured workers in returning to regular activity and work, and primary care practitioners play a key role in this process.
A new clinical practice guideline for concussion, published in 2024, provides valuable guidance for primary care practitioners on the assessment, diagnosis, and management of concussion, such as those that are work-related. Additionally, new legislation for BC employers and workers aims to ensure that individuals can return to work safely and in a timely manner following any workplace injury, such as a concussion. Further information on supporting patients’ return to work and additional resources for managing work-related concussion are outlined in the BC Medical Journal article.
Youth suicide and self-harm by medications in BC: The role of means restriction (November 2025)
Authors: Brandon Yau, Mojgan Karbakhsh, Megan Oakey, Jeffrey Trieu
This article by authors from Vancouver Coastal Health, BC Centre for Disease Control (BCCDC), and BCIRPU highlights the role of means restriction – an evidence-based intervention – in limiting access to medications to prevent youth suicide and self-harm. The article presents data that show that poisoning is the leading cause of hospitalizations for intentional self-harm among youth, particularly among females. It also identifies the most common medications involved in youth intentional self-poisoning, which includes commonly prescribed medications and over-the-counter medications.
These findings underscore important opportunities for prescribers, policymakers, and the public to help reduce the risk of intentional self-harm and suicide among youth through a range of potential actions. Read more about the article and the actions in the BC Medical Journal.
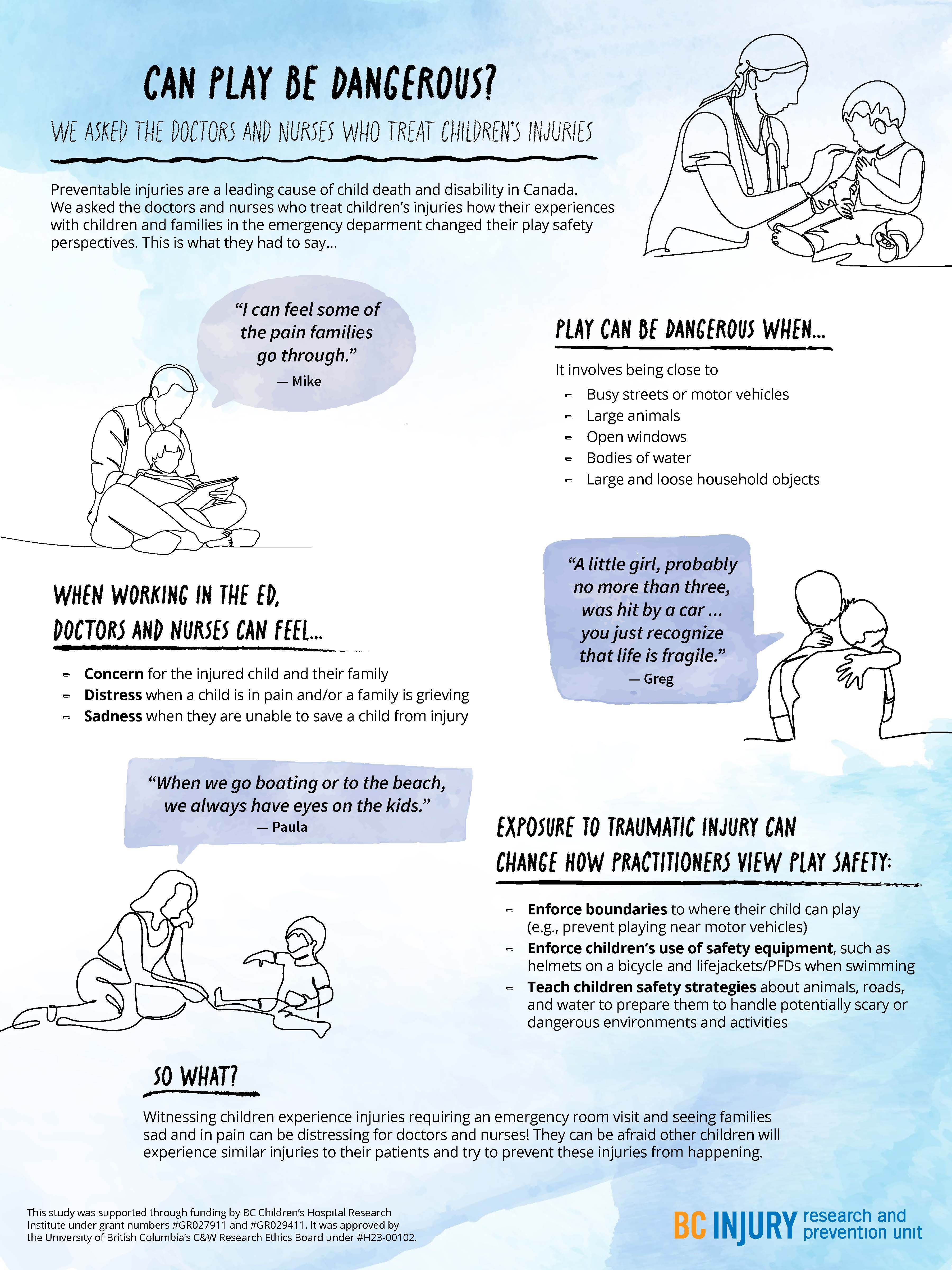
- distress when a child was in pain and when a family was grieving; and
- sadness in the event they were not able to save a child in their care.
- concern for the injured child and the child’s family;
Particularly traumatic events, such as those involving vivid sights and sounds (e.g., families holding each other and having extreme reactions), stuck with the practitioners, having long-lasting impressions on them and causing them to re-live these events in the years following their exposure.
Even after their shift was over, practitioners said that they changed how they approached parenting and how they perceived safety during play as a result of witnessing these traumatic events. They reported having more knowledge of the causes and consequences of severe injuries, such as those that require hospitalization or emergency care. For example, practitioners were more likely to enforce boundaries around where their children could play, such as by forbidding their child to play near busy streets. They also were more likely to tell their child about safe play environments and equipment, and put this equipment on their child before play, such as explaining the benefits of using helmets while riding bikes.
Practitioners were more likely to enforce boundaries around where their children could play, and use safety equipment, such as bike helmets.
Practitioners also described being concerned about their children’s play near open windows, around large bodies of water unsupervised, and in environments where firearms were present. They also expressed worry about their children’s play on trampolines and on motorized vehicles, such as ATVs. Findings related to trampoline play safety concerns were published in the journal Injury Prevention.
Observing family grief due to child injury or death affected the mental well-being of health care practitioners, drawing attention to the need for mental health supports for those involved in caring for severely injured and dying patients.

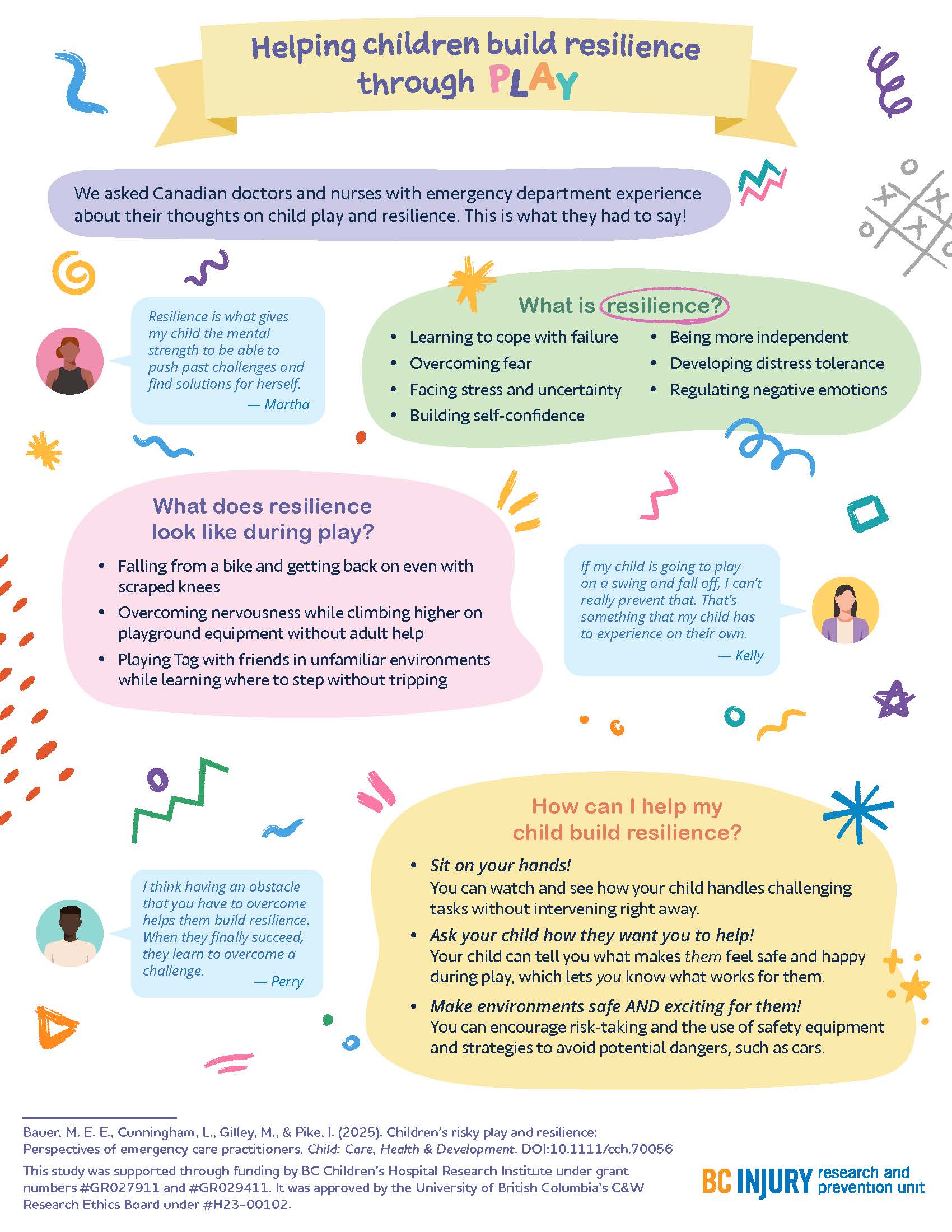
"Raise more resilient children through play...watch and see how your child handles challenging tasks without intervening right away." —Dr. Michelle Bauer
Building resilience through play
How can parents help their children build resilience? By letting them play!
The experiences that practitioners witnessed encouraged them to support their children in building resilience through play; specifically, by supporting children in learning to cope with failure, overcome fear, build self-confidence, develop distress tolerance, and regulate negative emotions. Findings related to building resilience through play were published in the journal Child: Care, Health, and Development.

Parents fostered resilience in their kids by:
- helping their kids get back on bikes after they fell off and wanted to try again;
- sitting on their hands so they did not instinctively reach for their children when their children fell down; and
- encouraging participation in challenging and thrilling activities in forests and water while safety equipment was used.
"There are a few ways that parents can raise more resilient children through play that are supported by literature and our study findings," said Dr. Bauer. "One: watch and see how your child handles challenging tasks without intervening right away."
"Two: Ask your child how they want you to help—let them tell you what makes them feel safe and happy during play. Let them lead. And three: make play both safe and exciting by encouraging risk-taking, teaching them how to avoid hazards, and using safety equipment.”
This research was supported through Drs. Bauer’s and Gilley’s receipt of a clinical and translational research seed grant from the BC Children’s Hospital Research Institute (BCCHR), Dr. Bauer’s BCCHR postdoctoral fellowship award, and additional training provided to Dr. Bauer through her participation in the Programs and Institutions Looking to Launch Academic Researchers (PILLAR) program through ENRICH, a national organization training perinatal and child health researchers.
Learn more about the study through two infographic posters:
Graphics and posters by Milica Radosavljevic